Fundamentals of Fluorescein Angiography
|
|
Abnormal Angiographic Hypofluorescence Hyperfluoresence |
Hypofluorescence
Hypofluorescence is defined as an absence or reduction of normal fluorescence. Hypofluorescence is the result of either blocked fluorescence or vascular filling defects. Blocked retinal fluorescence is most commonly caused by superficial or intraretinal hemorrhages. Choroidal fluorescence can be blocked by the anterior deposition of abnormal materials such as blood, lipid exudates, lipofuscin, xanthophyll or melanin. It is important to differentiate this type of choroidal hypofluorescence from the normal attenuating effect of the retinal pigment epithelium. It is often possible to determine the histologic location of the blocking structure based on the visibility of blood vessels. Preretinal hemorrhages, for example can block the visibility of both the retinal and choroidal vasculature while subretinal blood would only obscure the choroidal circulation.
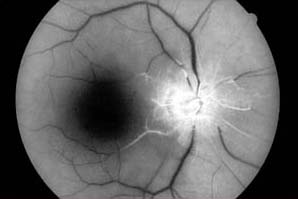
 Blocking Defect from Superficial Retinal Hemorrhages |
 Vascular Filling Defect Central Retinal Artery Occlusion |
Hypofluorescence can also be the result of vascular filling defects. Inadequate circulation will cause the affected vessels to appear darker than expected. Vascular occlusions can cause a delay or decrease in perfusion that appears hypofluorescent. Capillary nonperfusion is a common finding in diabetic retinopathy. Filling defects can also occur in the optic nerve head as a result of atrophy or ischemia. It is important to understand the relationship between hypofluorescence due to filling defects and the specific phase of the angiogram. In many vascular occlusions, hypofluorescence is a temporary finding until delayed filling of the affected vessel occurs.
Hyperfluorescence
Autofluorescence and psuedofluorescence are terms to describe the appearance of apparent hyperfluorescence in the absence of fluorescein. Autofluorescence refers to recordable hyperfluorescence that is believed to occur naturally in certain pathologic entities such as optic nerve drusen and astrocytic hamartomas. Some, but not all drusen appear to fluoresce under the excitation wavelengths used for fluorescein angiography.
Pseudofluorescence can occur as a result of crossover in the spectral transmission curves of the exciter and barrier filters. When crossover is present, reflectance from bright fundus structures will not be fully blocked by the barrier filter. Crossover can be the result of mismatched or aging filters. Modern interference filters rarely exhibit significant crossover unless they have deteriorated. Control photographs taken before injection of fluorescein are used to detect the possible presence of pseudofluorescence.
Transmission defect. Depending on the density of retinal pigmentation, background fluorescence from the choroid can be visible as hyperfluorescence in the angiogram. A 'window defect' is an area of hyperfluorescence that occurs when there is an absence of pigmentation due to damage of the pigment epithelium. The absence of pigment allows a view of the underlying choriocapillaris. Window defects remain uniform in size throughout the angiogram. Their brightness rises and falls with the choroidal fluorescence. It is important to differentiate hyperfluorescence due to transmission defects from leakage.
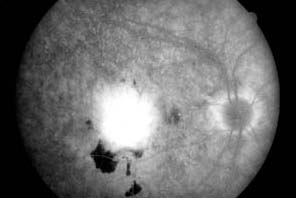
Major choroidal vessels appear hyperfluorescent
through a "window defect" in the retinal pigment epithelium
Leakage is hyperfluorescence due to the active focal leakage of fluorescein into retinal tissues or the vitreous cavity. Any leakage of fluorescein from a retinal vessel or within the retinal tissues indicates an abnormality. It is often the result of a breakdown or lack of tight vascular junctions in abnormal blood vessels. Retinal neovascularization can occur in any retinal condition that causes ischemia such as diabetic retinopathy. If present, retinal new vessels leak progressively throughout the angiogram.
Choroidal, or subretinal neovascularization will also leak fluorescein. These blood vessels originate in the choriocapillaris and can be found in any condition that causes breaks in Bruch's membrane. Choroidal new vessels are a common finding in age related macular degeneration and can be sight threatening. Fluorescein angiography is valuable in identifying the location and extent of choroidal neovascular membranes.
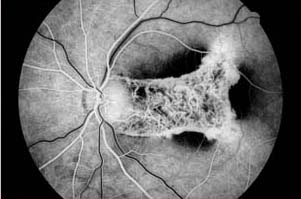
 Leakage from a choroidal new vessel membrane, macular degeneration |
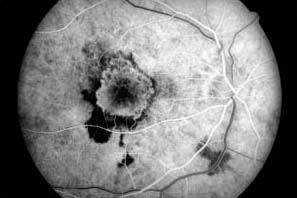
 Late phase photograph of the same eye demonstrates continued leakage |
Capillary microaneurysms, retinal telangiectasias, arterial macroanuerysm, papilledema and some vascularized tumors will also exhibit leakage. Leakage can lead to late staining or pooling of dye.
Staining refers to late hyperfluorescence that is the result of leakage which diffuses into certain tissues. Perivascular staining in vein occlusions and diabetic macular edema are common examples. Drusen and chorioretinal scars can also exhibit staining. Normal staining can occur in the optic nerve and sclera as a result of normal choroidal leakage. Scleral staining is usually only visible when there is a reduction or absence of the pigment epithelium and the sclera can be seen clinically.
Pooling is the accumulation of dye within a distinct anatomic space. Pooling can occur in serous detachments of the sensory retina or the retinal pigment epithelium due to a breakdown of the blood/retinal barrier. Central serous chorioretinopathy is a condition that often demonstrates the pooling of fluorescein leakage.
